Alzheimer’s disease, a progressive neurological disorder, stands as the most common cause of dementia. In 2023, an estimated 6.7 million Americans aged 65 years or older had Alzheimer’s disease. In Alzheimer’s, neurons in the memory-related regions in the brain, such as the hippocampus and amygdala, as well as other cognitive areas lose function and eventually die. Some common characteristics as a result of this neuronal damage are memory loss, difficulties in learning and communicating, and changes in behavior.
Understanding the Pathological Features of Alzheimer’s Disease
Alzheimer’s disease occurs because neurons lose the ability to communicate with one another. It primarily occurs due to two key pathological features: amyloid plaques and neurofibrillary tangles.
- Amyloid Plaques: In normal neurons, a protein called amyloid precursor protein (APP) is processed into fragments that help with normal cell function. Whereas in Alzheimer’s disease, this protein is processed abnormally, resulting in the formation of sticky peptides called beta-amyloid. These beta-amyloid peptides accumulate in the extracellular space, forming clumps called amyloid plaques which inhibit the electrical and chemical connections between neurons. As the pathways are blocked, communication between neurons is hindered, leading to cognitive dysfunction and symptoms characteristic of Alzheimer’s disease.
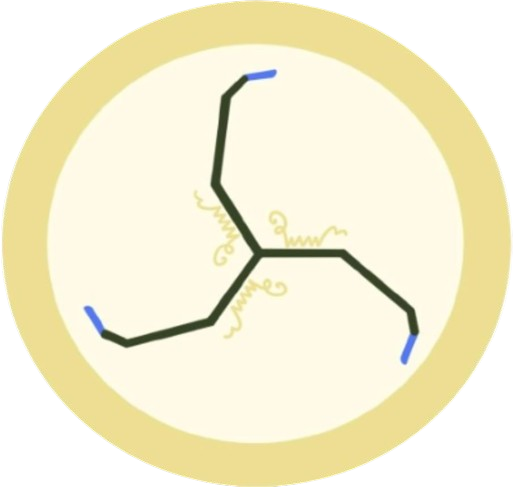
- Neurofibrillary tangles: Within healthy neurons, microtubules and tau protein form ordered structures that transport ions and nutrients within the cell. In Alzheimer’s disease, chemical changes within neurons damage the tau protein and cause microtubules to wrap abnormally, forming neurofibrillary tangles, which block the transport of ions and nutrients into the cell.
As plaques and tangles grow within brain tissue, neuronal connections decrease and malnourished cells lose function, leading to widespread neuronal death, loss of brain mass, and severe cognitive impairment.
Risk Factors and Symptoms of Alzheimer’s Disease
Understanding the risk factors for Alzheimer’s is crucial for early detection and effective management. Here are some common risk factors associated with Alzheimer’s:
- Age — Older age is the greatest known risk factor for Alzheimer’s disease. Risk increases significantly after age 65.
- Family History — Individuals who have a family history of Alzheimer’s disease are at a higher risk of developing the condition.
- Lifestyle Factors — Factors such as smoking, physical inactivity, poor diet, and obesity have been linked to an increased risk of Alzheimer’s disease.
- Down Syndrome — People with Down syndrome are at a higher risk of developing Alzheimer’s disease.
- Head Trauma — Previous head injuries, especially those involving loss of consciousness, may increase the risk of Alzheimer’s disease later in life.
Some symptoms indicative of early or late stages of Alzheimer’s disease include:
- Apraxia: Difficulty executing specific motor movements.
- Aphasia: Have a hard time understanding or creating speech.
- Agnosia: Unable to recognize objects, people, and their senses.
- Amnesia: Loss of memory
- Anomia: Unable to recall names of people or objects.
Treatments
While there is no cure for Alzheimer’s, current treatments include cholinesterase inhibitors, which slow down the breakdown of acetylcholine — a neurotransmitter crucial for memory and learning — and anti-glutamatergic medications, which regulate the activity of glutamate — another neurotransmitter essential for memory and learning — by blocking excessive glutamate binding to neurons, thus preventing neuronal dysfunction and death.
In conclusion, Alzheimer’s remains a disease that affects many individuals and families throughout the world. As research progresses and awareness increases, there is hope for improved treatment and ultimately, prevention.
-Anushka Jain, Co-Founder, NernstNaK
Sources:
- https://youtu.be/TgrTchmo-uk?si=kQhCVPC2bW6gwt5m
- https://www.alz.org/alzheimers-dementia/what-is-alzheimers
- https://youtu.be/lql93382Hv8?si=X2eTaDru-UkptVPq
- https://youtu.be/wfLP8fFrOp0?si=n49a-z1fwLnvXJ3_
*Disclaimer: This article has also been posted to our Medium. NernstNaK is the rightful owner of this work on both our website and Medium, and thus stresses that there has been no plagiarism or copying on either account.*